Health and Disease: Process of Phagocytosis and Defences in the Body
| ✓ Paper Type: Free Assignment | ✓ Study Level: University / Undergraduate |
| ✓ Wordcount: 8258 words | ✓ Published: 06 Jun 2019 |
Health and Disease
Access to pharmacy
Q3 (3.2)
Explain the process of phagocytosis using a series of labelled drawings. Justify phagocytosis as a defence mechanism?
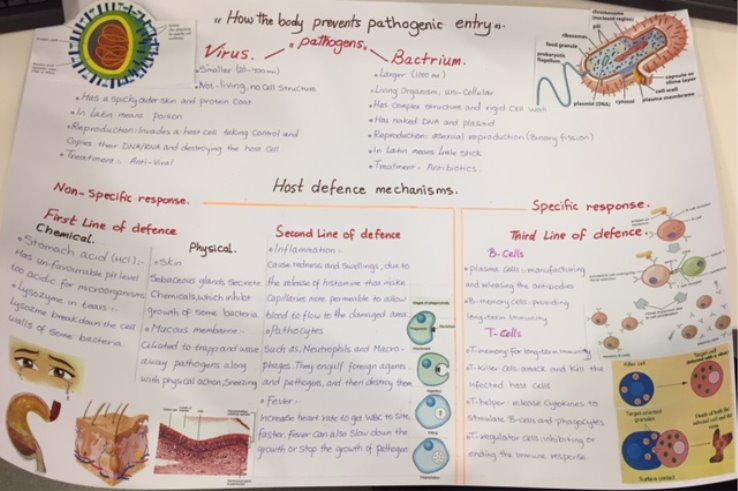
Pathogenic organisms such as bacteria and viruses need to enter the body of their host before they can cause harm. Evolution by natural selection has selected hosts adapted to defend themselves against such invasions. The body possesses many mechanisms that have evolved to prevent of pathogenic organisms include the non-specific defences and the specific defences. The non-specific defences consists of the primary line of defence and the secondary line of defence, so if the primary line of defence fail in preventing the entry of any pathogen the secondary line of defence will take the responsibilities to prevent them from gaining a foothold in the body and destroy them if they penetrate to the deeper tissues.
The blood consists of fluid called plasma that contains different constituents such as red blood cells or erythrocytes, white blood cells (WBC) or leukocytes and platelets. The mechanisms are related to the defence mechanism of body provided by white blood cells (WBC) or leukocytes. The leukocytes are divided into granulocytes and agranulocytes on the basis of granules (are tiny sacs containing enzymes that digest microorganisms) in their cytoplasm. Granulocytes contain three types of blood cells (neutrophils, basophils and eosinophil) and agranulocytes contain two types of cells (lymphocytes and monocytes).
After infection the number of WBC increase in the blood during the initial phase of infection. At this stage they are phagocytic in nature. Phagocytosis is specialised white blood cells in the blood and tissue fluid of non-specific secondary line of defence that refers to engulfing of large, solid particles often the engulfed particles are pathogens and destroy them. The stages of the phagocytosis are:-
- Stage 1 : Activation of the phagocyte; resting phagocytes are activated by the inflammatory mediators such as bacterial products like bacterial protein, capsules and acids,etc. It is also activated by complement proteins, inflammatory response. The inflammation is a non-specific response to any trauma occurring to tissues and can be controlled by chemical substance called histamine released when the tissue is infected to increase the capillary permeability, enable the phagocytic white blood cell such as neutrophils and monocytes to enter the infected area. As a result, the circulating phagocytes produce surface glycoprotein receptors that increase their ability to adhere the inner surface of capillary walls, enabling them to squeeze out of the capillary and be attracted to the site of infection.
- Step 2 : chemotaxis of phagocytes; chemotaxis is the movement of phagocytes towards an increasing concentration of some attractant such as bacteria l products (capsules, bacterial protein and acid) and phospholipids released by injured host cells or towards particular Chemical . Some microorganisms such as influenza a viruses, mycobacterium tuberculosis blocks the chemotaxis .
- Step 3:- Attachment of the phagocyte to the microbe ; attachment of microorganism is necessary for ingestion as the phagocytosis won’t happen unless the cell is in physical contact with the particle it wants to engulf. The cell surface receptors used for the phagocytosis depends on the type of the cell that is going the phagocytizing and the most common ones are opsonin receptors and antibodies. The opsonins are protein molecules that attach to the antigens on the surface of the pathogen. Some opsonins are not very specific so they can bind different pathogenic cells. The opsonins role is to enhance the ability of the phagocytic cells to bind and engulf the pathogen. The process of enhanced attachment is also opsonisation.
- Step 4 :- ingestion; after attachment the plasma membrane of phagocyte extends short projections known as pseudopods which engulf the foreign materials or microorganisms. This process is known as ingestion and during the ingestion, an electron pump brings proton (H+) into the phagosome. This lowers the pH within the phagosome to 3.5-4.0 so that when a lysosome fuses with the phagosome. This is the optimum pH for the acid hydrolases to effectively break down cellular protein. The acidification also releases enzymes that can kill microbes.
- Step5:- Digestion; phagocytes contain membranous sacs known as lysosomes produced by the Golgi apparatus that contains digestive enzymes called hydrolytic enzymes and bacterial chemicals. So after engulfment phagosome comes in the contact with the lysosome a single layered large structure is formed which is known as phagolysosome. The pathogen or the foreign materials are destroyed by the contents of phagolysosomes within 10-30 minutes.
- Step 6:- Egestion; the microbial fragments and the dead phagocyte is eliminated from the cell and collected in an area of infection to form pus.
The granulocyte (neutrophils) and the agranulocytes (monocytes) are two types of the specialised phagocytosis cells.
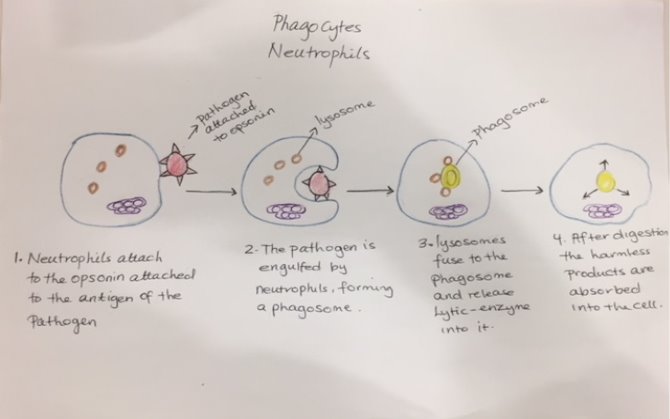
The neutrophils are the most abundant type of granulocytes and the most common phagocytes that are formed from stem cells in the bone marrow. They are travel in the blood and often squeeze out of the blood into tissue fluid. The neutrophils are recognised by their multi-lobed nucleus and are short-lived, but they are released in large numbers as a result of an infection. The neutrophils bind to the opsonin attached to the antigen of the pathogen then the pathogen is engulfed by the phagocytosis forming a phagosome. The neutrophils contain large number of lysosomes so the lysosomes fuse to the phagosomes and release the hydrolytic enzymes into it to digest the microorganisms. After digestion the harmless products can be absorbed into the cell. The neutrophils usually die soon after the digestion of few pathogens so the dead neutrophils are collected in the infection area to form pus.
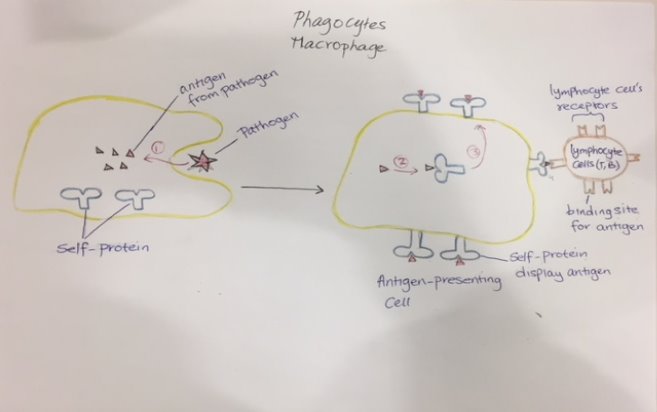
The monocytes are agranulocyte type of specialised phagocytosis white blood cells. Monocytes are formed in bone marrow from pluripotent stem cells; their direct precursor cell is promonocyte that derives from the monoblast. The monoblast cells divide and mature into monocytes in the bone marrow. Then monocytes enter the blood circulation and present in the blood vessels for relatively long time. After they migrate to the lymph nodes which are a network of major sites of B and T lymphocytes and other WBC, present in the body tissues. Most of the monocytes are present in lymph nodes where they mature and enlarge in size to become macrophages. Macrophages are specialised large phagocytic cells of the immune system that are formed in response to an infection or accumulating damaged or dead cells. The macrophages are playing an essential role in initiating the specific responses to invading pathogens, as they release chemicals called monokines to stimulate the B-lymphocytes to differentiate and release antibodies. The macrophages are phagocytic cells they attach to the pathogen and engulf them but they do not digest the pathogen fully. The antigen from the surface of the pathogen is not digested by the macrophages so it is saved. So it moves to a special protein complex on the surface of the cell that insures the antigen is not mistaken for a foreign cell. The cell becomes an antigen-presenting cell. The antigen-presenting cell exposes the antigen of the pathogen moves around the body where it can come into contact with specific cells that can activate the full immune response. So the other cells of the immune system such as T and B lymphocytes can recognise the antigen of the pathogen in the Antigen-presenting cell. These antigen-presenting cellshave an important role to increase the chances for antigen and immune cells to contact.
Q4 (3.1,3.3,4.4)
- Explain the process of the blood clotting and justify how it is a defence function.
The body is covered by the skin, which is the main primary first line of defence and for the skin to be protective it must be complete. Lacerations or abrasions damage the skin and injury the blood vessel. When this occurs, the body open to infections and loss a lot of the blood. The body must prevent the excessive loss of blood by the formation of clots, making a temporary seal to prevent infections, and repairing the skin. Blood clotting, which is also known as coagulation is a complex process to prevent excessive blood loss by forming clots but also to make sure that these clots are not be formed in the blood vessels where they are not needed.
There are several process involved in clotting of the blood so when the blood vessel is injured, the walls of the blood vessel contract to limit the flow of the blood to the damaged area. Then a small blood cells called platelets stick to the site of injury and spread along the surface of the blood vessel to stop bleeding. At the same time, chemical signals known as granules are released from small sacks inside the platelets; this process is known as secretion. These signals will attract other platelets cells to the area of injury and make them clump together to form what is called a platelet plug, this process known as aggregation. On the surface of these activated platelets, there are calcium ions and at least 12 factors known as clotting factors. The clotting factors are proteins that activate an enzyme cascade and working together in series of complex chemical reactions called coagulation cascade; where the thrombokinase enzyme change the prothrombin to thrombin in the presence of calcium ions. Thrombin combines with soluble fibrinogen found in the blood and forms insoluble fibrin. The insoluble fibrin forms thread like structures that form a sticky mass and this forms a network of a sticky substance at the cut or the damage area of the blood vessel. This sticky mass on the cut becomes denser and denser and is known as clot and act as mesh to stop the bleeding.
The coagulation factors flow in the blood in an inactive form, but when blood vessels injured is secrete a substance called thromboplastin which initiates the reactions that result the formation of the clots.
Once the clot has formed, it begins to dry out and form scab. As the scabs dries, it shrinks and drawing the sides of the cut together to make a temporary seal, under which the skin is repaired. The first step is the deposition of fibrous collagen under the scabs. The epidermis layer contains stem cells which are undifferentiated so then they divide by mitosis division and migrate to the edge of the cut where there they become specialised into new skin cells. New blood vessels are also formed to supply the new tissues with oxygen and nutrients. Later the tissues formed contract to help draw the edges of the cut together so that the repair is complete and as the new skin is formed the scabs are released. This process called skin repair.
- Differentiate between the role of B and T- lymphocytes, using diagrams (attached to the assignment)
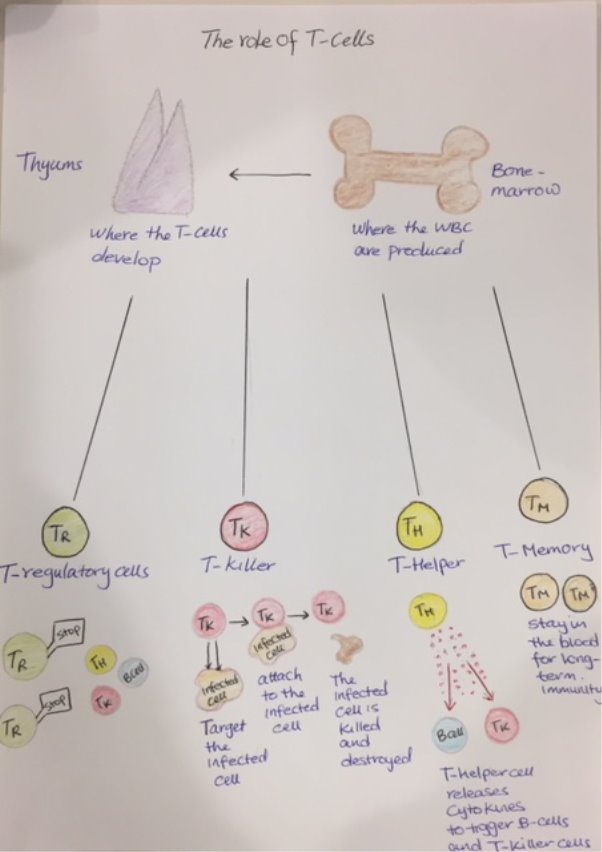
Lymphocytes are a-granulocytes type of the white blood cells in the specific third line of defence, which produced in the bone marrow but after the production they leave the bone marrow. Some of the lymphocytes travel to thymus where they develop and become specialised into subset of T-lymphocytes cells; each have different function. While the other lymphocytes travel to lymphoid tissues like lymph nodes, where they develop and become specialised into B-lymphocytes cells. Although both types of lymphocytes (T and B cells) have a large nucleus and specialised receptors on their surface membrane, identify the invaders and attack (specific immune responder), and both produced in bone morrow, they mature in different places and they play different roles in helping the body to eliminate microorganisms.
The role T-cells :-
After T-cells develop in the thymus, they differentiate into four main types which are T-killer, T-helper, T-regulator and T-memory cells; each of them has an important function in the immune system. They are either travel around in the blood or lymphatic system or migrate to different organs in the body. But as soon as a specific pathogen with its specific foreign antigen molecules on its surface stimulate the immune system, the immune system start to make the T and B cells to recognize and attack the specific antigen in the pathogen; only certain T and B cells can match and react to a specific antigen.
The helper T-cells release chemicals messengers known as cytokines to trigger the B-cells to develop and differentiate into plasma cells to release antibodies, and also stimulate the phagocytosis by phagocytes. The helper T-cells release also interferon which inhibit the pathogen such as virus replication and stimulates the activity of T-killer.
The T-killer cells will target, attack and kill host-body cells that have become infected by invader or display foreign antigen or are cancerous. Natural killer T cells also produce chemicals known as interleukins that can stimulates the clone expansion of memory T cells. They also release other chemicals to help regulate the immune response and protect against the invaders and tumours.
Regulatory T-cells are also called tregs; T regulatory cells were originally identified as a CD4+CD25+ T cell population with the capacity to stop T-lymphocytes immune response. This is because the T-regulatory cells develop and their CD4 and CD25 cell surface proteins markers are up regulated. The treg cells would effectively stop an immune response after it has begun. This helps to control the immune reaction and shut the immune response after the pathogen has been successfully eliminated to prevent autoimmunity. Autoimmune disease occurs when the immune system start to attack our own normal antigen, possibly because these antigen that are not normally exposed become exposed to attack.
Memory T cells stay around for a long time after immune response has finished providing long-term immunity. In this way they can react quickly without symptoms if the same pathogen appears again and also they multiply to produce a large number of T-cells to remove the pathogen.
The role of B-lymphocytes cells
The B-lymphocytes develop in lymph nodes and travel in the blood. When they come across pathogen the B cells are stimulated. The T-helper release cytokines to stimulate the B-cells into action to produce plasma cells and memory B-cells. Unlike T-cells, B-cells cannot directly attack infected cells. Instated the plasma cells primarily produce proteins called antibodies.
The plasma cells; each plasma cell is specialized to produce a particular antibody – antibody is a specialised protein with receptor that are complementary bind to a specific antigen. The role of the antibodies is to act as flag on the infected cell so they can easily be recognized by the specialized cells such as T-cells or phagocytes that are responsible for engulf the infected cells and destroy them. The plasma cells disappear after an immune response is complete, memory B cells stay circulating in the body for long time.
The B-memory cells stay in the body for a number of years for faster response without any symptoms if the same pathogen again, the right antibodies are directly produced to help fight them off.
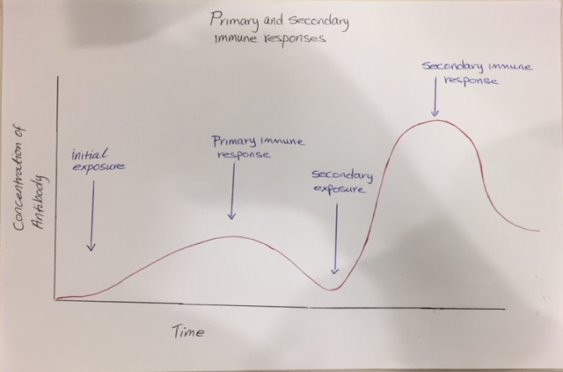 As it shows in the graph, when a person is exposure to an infection for the first time, the concentration of antibodies are very low, but in meantime the B-cells are produced and differentiate into plasma cells to produce the right antibodies for that pathogen; so slowly the number of antibodies is increasing to fight the pathogens, here the person is experience the symptoms and it takes few days to cure. After the infection, the B-cells produce B-memory cells to stay around in the blood for long-term immunity. Later when a person is exposure to the same infection, the immune system will responses very quickly, as the B-memory cells will immediately provide the right antibodies to fight the pathogens, it will provided in large number, therefore the concentration of antibodies will rise up, here the person will not experience any symptoms and won’t take long to cure from the infection.
As it shows in the graph, when a person is exposure to an infection for the first time, the concentration of antibodies are very low, but in meantime the B-cells are produced and differentiate into plasma cells to produce the right antibodies for that pathogen; so slowly the number of antibodies is increasing to fight the pathogens, here the person is experience the symptoms and it takes few days to cure. After the infection, the B-cells produce B-memory cells to stay around in the blood for long-term immunity. Later when a person is exposure to the same infection, the immune system will responses very quickly, as the B-memory cells will immediately provide the right antibodies to fight the pathogens, it will provided in large number, therefore the concentration of antibodies will rise up, here the person will not experience any symptoms and won’t take long to cure from the infection.

- Explain the essential difference between humoral and cellular responses as shown by B and T –lymphocytes.
The immune system distinguishes two groups of foreign substances. One group consists of antigens that are freely circulating in the body; these include molecules, viruses and foreign cells. The other group consists of antigens tagged with the cellular surface protein called MHC; the MHC proteins found on the surfaces of cells that help the immune system recognize foreign substances. can initiate from antigens that have been engulfed but without being fully destroyed (antigen is saved and exposed) .Depending on the kind of foreign invasion, two different immune responses occur; the humoral response (or antibody-mediated response) and the cell-mediated response.
The cell-mediated response ; involves the phagocytes and T-cells but mostly T-cells and respond to any cell that display MHC protein, including cells invaded by pathogens and tumour cells. The steps of events for the cell-mediated response:-
- Antigen-presenting cells displaying the antigen of a pathogen to T cells
- T-helper cells release interleukins to stimulate the activation of T-cells
- If the MCH and endogenous antigen (virus‐infected cells that are actively synthesizing foreign proteins) are displayed on the plasma membrane, the T-cells divide, multiply, and differentiate into T-killer cells. The T-killer cells attack and kill the cells displaying the antigen.
- If the MHC and exogenous antigen (antigens that have been engulfed and broken down) are displayed on the plasma membrane, the T-cells divide and produce T-helper cells. The T-helper cells produce chemical called cytokines to stimulate the cells to produce antibodies that bind to the antigen and also stimulate the phagocytes cells to engulf and destroy the antigen.
The humoral response:- (‘’humor’’ is a term for body fluid used in medieval) is the immune response that involves the B-cells that recognize the antigen of the pathogen that are circulating in the blood. The steps of the humoral response:-
- T-helper cells release cytokines to stimulate the B-cells, in some cases, both the chemical messenger and the antigen in the pathogen are required to activate B-cells and start the B-cells division.
- B-cells divide and differentiate into plasma cells that release antibodies with receptors complementary to the antigen receptor in the pathogen so they circulate around the body, binding to the antigen.
- B-cells produce memory cells that can provide long term immunity.
Q5 (4.1)
Explain antigen and antibody interaction. Use diagram (attached to the assignment)
Antigens are molecules that can stimulate the immune response. Almost any molecule could act as antigen, but they are usually protein or glycoprotein in the plasma membrane of the pathogen; such as bacteria, viruses or fungi that cause infection and disease. Foreign antigen will be detected by the immune system and will activate the production of antibodies. Antibodies is also called immunoglobulin, are complex protein manufactured by the plasma cells in the immune system. They are released in response to an infection in order to fight against foreign antigens. Antibody molecules are typically Y-shaped with a binding site on each arm and have two distinct regions, which are variable region that have specific shape to the shape of antigen, the other region is the constant region that is same for all antibodies. The binding sites of each antibody have specific shape that is complementary to a particular shape of antigen. Means only antigens that match this shape will fit into them. Therefore the immune system must manufacture one type of antibody for every antigen that is detected. The function of antibodies is to complementary bind to particular antigens and inactive them so that other immune cells can take over, destroy and eliminate theses foreign antigens. This is the specific chemical interaction between the antibodies and the antigens during immune reaction, and is the fundamental reaction in the body by which the body is protected from complex foreign molecules.
Antibodies work in different ways, but most act by attaching to the antigen on the pathogen. There are three main group of antibodies; the opsonin, agglutinins and anti-toxins.
Opsonins are group of antibodies that bind to the antigen so then they can act as binding sites for phagocytic cells to make them more adherent to phagocytic cells and more amenable to engulfment or ingestion. Some of opsonins are non-specific and can attack any type of pathogen, but the some opsonins are specific and bind to very specific antigen.
Agglutinins; as each antibody molecules has two identical binding sites, it can crosslink the pathogens by binding to an antigen on one pathogen in one binding site and the other binding site can bind to another antigen on another pathogen . When antibodies perform the crosslink of pathogens they agglutinate (clump together) pathogen, this inhibit the function of antigen and are readily engulfed by phagocytes.
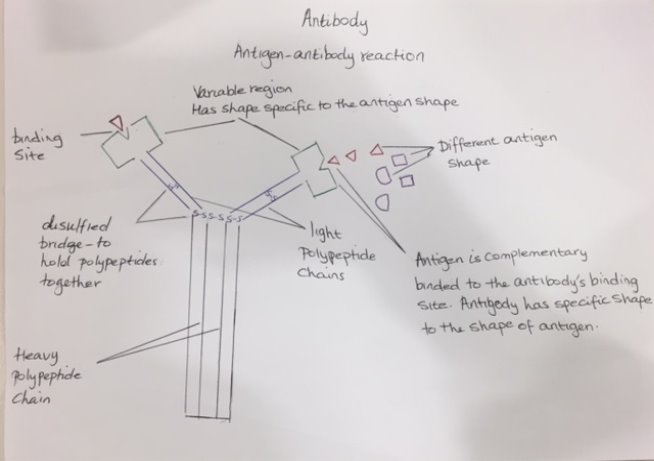 Anti-toxin; pathogen cells are release molecules that may be toxins so some antibodies called anti-toxins will bind to the toxin molecules produced by the pathogen and renders them harmless.
Anti-toxin; pathogen cells are release molecules that may be toxins so some antibodies called anti-toxins will bind to the toxin molecules produced by the pathogen and renders them harmless.
Q6 (4.2,4.3)
- Write a short explanation, which explain the difference between natural/acquired immunity and active/passive immunity
- Immunity can be achieved naturally or artificially. Natural immunity is gained through normal life process. Artificial immunity is gained through medical intervention. The immunity can also be achieved actively or passively. Actively immunity is gained when the immune system is activated and manufactures its own antibodies. Passively immunity is gained when the antibodies are supplied from another source.
| Naturally immunity | Artificially immunity | |
| Active | Active naturally immunity refers to immunity, which results from the production of antibodies by the person’s own immune system in response to a direct contact of an antigen. Antigens enter the body naturally; the body’s own immune system induces specialized lymphocytes (T-cells and B-cells) and antibodies. example immunity gained through illness and recovery such as immunity to chickenpox | When an antigen is entered the body artificially, by the vaccine so the body induces an immune response to produce lymphocytes cells; to activate the immune system to produce the B-memory cells and T-memory cells so when the same antigen enter the body are ready to fight it. Example a person is injected with a weakened, dead or similar pathogen so this can activates the person immunity system such as immunity to TB and influenza. |
| Passive | Antibodies are provided from the mother to the foetus via placenta or infant via the mother milk. This makes the baby immune to diseases to which the mother is immune. It is important in the first year of the baby’s life till he/she develop their own immune system/. | Refers to a short-term immunity which results from the induction of antibodies from the outside. Preformed antibodies in the immune serum are introduced by injection. Means that the injection of antibodies made by another individual. Example; tetanus can be treated in this way when the vaccination using toxoid did not work. |
- Explain the basis of immunisation
According to world health organisation (WHO) Immunisation is the process whereby an individual is made immune or resistant to an infectious disease, this can be achieved by receiving vaccination usually in the form of an injection. Vaccines stimulate the body’s own immune system to protect the person against subsequent infection or disease and provide immunity to that disease. This is can be done by inject antigenic material; the antigenic material can be harmless or weakened pathogenic organisms or it can be a dead one, so immune system will treats the antigenic material as a real disease. As result the immune system is activated and manufactures the specific antibodies to that antigen and also the memory cells. The memory cells will provide the long term immunity so when the antigen of real disease the plasma cells will produce the correct antibodies to kill it. This known as the second immune response, which provides a quick immune response and a large number of antibodies to fight the antigen without showing any symptoms. There are two applications of vacation that provide immunity, the herd vaccination and the ring vaccination. The herd vaccination is using vaccine to provide immunity to all or almost all of the population at risk. So when enough people are immune, the disease can no longer spread through the population and herd immunity is achieved. While the ring vaccination is used when a new case of disease is reported and involves vaccinating all the people in the immediate vicinity of new case.
Q7 (5.1)
Diabetes
Type:- metabolic disorder
Causes of disease:-
| Diabetes is a serious life-long health condition, in which the body’s ability to produce or respond to the hormone called insulin is impaired, leading to abnormal metabolism of carbohydrates and the blood sugar level become too high. There are three main types of diabetes; type1, type2 and gestational diabetes.
Type1 diabetes is a form of diabetes mellitus that typically develops in children and in young adults. Is thought to be an autoimmune disease; normally the immune system produce antibodies to attack the antigen of the pathogen but in autoimmune, the immune system makes antibodies that attack part of the body. So the type1 occurs when the antibodies produced attack the beta cell in the pancreases and destroy the cells that make insulin. Type 1 is caused by genes and environmental factors; the popular theory is that there is a virus that triggers the immune system to make these antibodies that destroy insulin-producing beta cells of the pancreas. Type2 diabetes is the most common type that occurs in people over age of 40, in south Asian there is a greater risk to occur from the age of 25. Type 2 usually starts with insulin resistance, a condition in which muscle, liver and fat cells do not custom insulin well. Leading to that the body requires more insulin to stimulate the cells of the body to absorb glucose out of the blood and also to convert the extra glucose in the blood to glycogen for storage in the liver. At first, the pancreas is able to makes more insulin to keep up with the added demand. But over time, the pancreas won’t be able to make enough insulin therefore the glucose level in the blood rise up. This can be caused by several factors such as genes and lifestyle factors. Lack of physical activity and overweight can cause insulin resistance and is common in people whose the location of the body fat is in the belly fat which is linked to insulin resistance, causing type 2 diabetes. Also having family history of diabetes makes it more likely to develop diabetes. Gestational diabetes is a type of diabetes that occurs during pregnancy especially during their third trimester caused by the hormonal changes of the pregnancy along with genetic and lifestyle factors, where the body cannot produce enough insulin to control the glucose absorption. This is because hormones produced by the placenta contribute to insulin resistance and most pregnant woman are unable to produce enough insulin to overcome insulin resistance. Also extra weight is linked to the gestational diabetes, as the women who are overweight may already have insulin resistance and when they become pregnant they gaining extra weight. |
The symptoms of the disease (Diabetes):-
Symptoms of type1 diabetes can develop very quickly, over a few days or weeks in children, while for adult it takes few months. Symptoms of type2 often develop slowly, over several years, and can be so mild that cannot even be noticed; some people have no symptoms or do not find out that they have the disease until they have diabetes-related health problems such as heart problems or blurred vision. The main symptoms of diabetes are polyuria (increased urination), polydipsia (thirst) and tiredness. Even the diabetes type1 is different to its counterpart type2 diabetes, but the major symptoms of the diabetes are similar for both types. Common symptoms for type1 and type2:-
There are symptoms that develop over many years-usually at least 10 years. They are relating to how blood glucose levels can affect blood vessels. High glucose level in the blood our uncontrolled blood glucose can, damage both the large blood vessels and the tiny blood vessels. Damage tiny blood vessels don’t deliver blood as well as they should cause micro-vascular complications; eye that can lead to damage to the retina in the eyes that cause loss of vision. , kidney that can cause kidney failure where the kidney will be unable to filter the blood. And nerve disease as the tiny vessels’’ feed’’ the nerve so if they are damaged then the nerve will also be damaged. While damaging the large vessels can cause macro-vascular complications that can lead to plaque eventually building up and potentially resulting to heart attack |
.
Treatment (Diabetes):-
| To prevent any short-term or long-term complications, the level of glucose in the blood must be controlled carefully by:-
Healthy diet; aim to eat diet low in fat, salt, sugar and diet high fibre and plenty of vegetables as broccoli. Some fruits contain high sugar content such as bananas, cantaloupes, dates, grapes, watermelon, pineapples, and oranges, while the other type of fruit such as blueberry, cherries and pear do not affect blood glucose levels and may also improve glucose control and insulin sensitivity over time. Regular physical activity; physical activity is highly recommended for a diabetic to reduce any risk of complications such as heart attack and vessels diseases. Example of some activity are cycling, jogging or even 30 min walking, dancing and swimming or any other activities that can gets the person mildly out of breath and mildly sweaty. The activities can either be a minimum of 30 minutes at least five times a week or spread the activity over the day. This can also help to lose weight, as overweight is one of the risk factor for diabetes so losing some weight will help. Taking medication; some medicine are taken after meals to help absorb the glucose from the blood such as metaphorin and glacizide. For type1 where the insulin are not produced, the insulin injections are needed for the rest of the life; as the insulin is not absorbed in the gut, it is needs to be injected rather than taken as tablets. The type of insulin advised will be tailored to a diabetic needs. Most hospitals and Gp have special diabetes clinics to give advice on diet and lifestyle, checking on progress and regular checks are also include such as checking the level of blood glucose, cholesterol and blood pressure, eye checks to detect problems with the retina and prevented from getting worse foot checks to prevent foot ulcers (is an open wound usually located in the bottom of the foot that can prone to infections), and urine and blood tests to indicate early kidney problems.
|
Alcoholism
Type:- human induced disease
Causes of disease:-
| Alcoholism has known as such as alcohol dependence as the body gradually becomes dependent on or addicted to alcohol, where alcohol becomes the most important thing in the life. Some people may drink too much alcohol and causes problems but there are not physically dependent on alcohol so this is referred to as alcohol abuse.
There are many causes of alcoholism include; Chemical Changes in the brain over time alcohol will alter brain chemistry; this is because when a person drink alcohol the brain produces dopamine that makes the person feels good. So the body builds up a tolerance to dopamine, which will increases the pleasurable feelings leading to that the person wants to drink more often even if it causes negative consequences or if it harm. Eventually these pleasurable feelings related to alcohol drinking so to prevent withdrawal of these feelings the person will be engage in drinking more and more otherwise the withdrawn of these feelings can be dangerous. Social and environmental growing up in society where alcohol is legal and socially acceptable, in most cases it is socially required and refusing it making people thinks that the person is abnormal. The pressure to drink can be huge specially if the person is being around heavy drinkers or living with an alcoholic, this increase the risk of developing the dependence on alcohol. Genetic; researcher states that is not only environmental factors play a role in alcoholism, the genetic and alcoholism is related. The people whose parents have or had alcohol drinking problem are more likely to develop alcoholism. Hereditary alcoholism is dangerous among those with alcoholic family member. |
The symptoms caused by the disease (Alcoholism):-
| Symptoms of alcoholism are based on the physical outcomes that occur as a result of alcohol addiction and on the behaviours.
People with alcoholism are engaging in these behaviours include;
Physical symptoms:-
Long-term complications; serious and lasting liver damage. The liver role is removing the toxins from the blood and when drinking too much the liver won’t be able to filter the alcohol and other toxins from blood stream. This lead to liver disease. |
Treatment (Alcoholism):-
| recovering from alcohol use disorder is hard but it depend on the person ability to stop drinking, some people think the only way to deal with it is with willpower as it is all on their own and depends on the situation and the goals they aim for. There is a combination of treatment that works best and can get all of them through a program. Some of these programs are inpatient or residential is where you can stay at a treatment centre for a period of time. Others are outpatients programs are where the patients live home and go to the treatment centre for treatment.
There are different medications that may help with alcoholism include: Naltreoxne; a drug works by blocking certain receptors in the brain that associated with alcoholic, this drug decrease the craving for alcohol. Acamprosate is a medication that can help to re-establish the brain original chemical state before alcoholic dependence; this drug must be combined with theory. A patient with liver damage must have liver transplant, but waiting list for liver transplant are long and the alcoholism has rarely chance to get it as there are some people how deserve it more and they haven’t damaged their liver by purpose. Before liver transplant the patients must write a contract that they stop drinking alcohol otherwise there is no point of transplant new liver to them as they may damage it again.
|
Leukaemia
Type: – Cancer
Causes of disease
| Leukaemia is a group of cancers; cancer of blood that begin in the bone marrow and result overproduction of abnormal white blood cells. These white blood cells are not fully developed and are called leukaemia. Leukaemia is common in children but it is most often occurs in adults over age 55. Leukaemia happens when the DNA of the immature blood cells, mainly white blood cells become damaged in some way. These causes the blood cells to grow and divide continuously, therefore that there are too many. Normally the healthy blood cells die after a period of time and are replaced by new cells, which are produced in bone marrow. But the abnormal blood cells do not die when they should; therefore they will be occupying more space. As more cancer cells are produced, they stop the healthy white blood cells from growing and functioning normally, by crowding out space in the blood.
There are some causes that increase the risk of leukaemia such as; Artificial ionizing radiation, viruses (i.e. T-lymphotropic and HIV), chemotherapy agents used in previous cancers, smoking. Some people appear to have a higher risk of developing leukaemia because of a fault in one or several genes so genetic predisposition can be a cause of leukaemia. Also people with down syndrome appear to have a higher risk of developing leukaemia due to a certain chromosomal changes. It has also been suggested that exposure to electromagnetic energy might be linked to leukaemia. |
The symptoms caused by the disease (leukaemia)
| Poor blood clotting:- As the bone marrow becomes full of abnormal cells, it is unable to make great number of normal blood cells which the body requires; this can lead to Poor blood clotting: too many Immature white blood cells will crowd out platelets, which are essential for blood coagulation. This can cause a person to bleed easily and restore slowly. They may also develop petechial, small red to purple spots on the body, indicating a minor haemorrhage.
Frequent infections: The white blood cells are important for combat off infection. If these are inhibited or not working properly, frequent infections can result. The immune system may attack other good body cells. Anaemia: the lack of good red blood cells grows, anaemia can result. This can involve hard or laboured breathing and pale skin as there are not enough red blood cells to carry oxygen to the body cells.
There are four main types of leukaemia;
|
Treatment (leukaemia)
| Treatment options will depend on the type of leukaemia and the person’s age and overall state of health. The main type of treatment is chemotherapy; which is used to kill the leukaemia cells or stop them from dividing. It is often given in circles of treatment and one cycle of treatment will consists of a series of doses of chemotherapy followed by break for the healthy cells to recover.
Radiation therapy which use a high energy radiation to kill the leukaemia cells. Cannot be used to all types of leukaemia. There is a treatment which activate the immune system to destroy these cells is known as biological therapy. Drugs can also be used to specifically recognize and kill these cells, this type of treatment called target therapy. |
AIDS
Type:- caused by pathogen(virus)
Cause of disease
| AIDS stands for Acquired ImmunoDeficiency Syndrome. So AIDS is a syndrome that caused by virus known as HIV, which stands for Human ImmunoDeficiency Virus. This disease affects the immune system, making individuals much more likely to get infections and diseases. AIDS is developed due to HIV infection, as the HIV is a retrovirus that infects the vital organs and the human immune system cells by attacking the immune cells called CD-4 cells, which are a subset of T-cells. T-cells are responsible to defend, kill and activate other immune cells, therefore when the virus progresses the number of T-cells begins to decrease causing the individuals unable to defend against any infections.
The virus progresses in the absence of antiretroviral therapy (is a drug therapy that slows or prevents the virus from developing), which means it is possible for a person to carry HIV without developing AIDS but without treatment the HIV can progress and gradually develop into AIDS. The rate of virus progression can varies from one to another depends on many factors such as the age ,the ability of the body to defend against the virus and the presence of infections , access to health care, individuals genetic inheritance. HIV can be found throughout all the tissues of the body but is transmitted through sexual transmission (having sex with someone who is HIV-positive without protection), fluid transmission (through blood by sharing and reusing syringes contaminated by HIV-infected blood) or by perinatal transmission ( a HIV-positive mother can transmit the HIV to her child during pregnancy and breastfeeding).
|
The symptoms caused by the disease (AIDS)
| The symptoms of HIV can vary from person-to-person and some people may not get any symptoms at all for many years. There are three main stages of HIV infection, with different possible effects.
Stage1; Acute primary infection; around 80% of people will experience symptoms a lot like normal flu such as fever, body rash, sore throat ,headache and joint stomach. A person can get these symptoms from the one to four weeks after becoming infected with HIV. The symptoms may not last more than two weeks. These symptoms can happen due to the reactions of the body to the HIV virus. Cells that are infected with HIV are flowing throughout the blood system. Therefore the immune system, in response, tries to attack the virus by producing HIV antibodies. This process is called seroconversion. Stage 2; the asymptomatic stage; which start when the seroconversion stage is finished, so many individuals start to feel better. In fact, the HIV virus may not expose any other symptoms for up to 10 or even 15 years (depending on age, background and overall health). However, the virus will still be active, infecting and attacking new cells and making copies of it. Over time this will cause a lot of damage to many immune cells. Stage3 : symptomatic HIV infection; By this stage of HIV infection there has been a lot of damage to the body’s immune system and many immune cells are infected. This means the body of individual is more likely to get serious infections or bacterial and fungal diseases that the immune system would otherwise be able to fight off. In this stage the AIDS has developed. Symptoms that you may have during the third stage can include:
|
Treatment (AIDS)
| Currently there is no cure and no vaccine for HIV but antiretroviral therapy treatment can stop the progression of the HIV and allow people opportunity to live a long and relatively healthy life, and reduces the risk of transmission. As the HIV treatment does not cure HIV, but it stops the virus from reproducing in the body. It can reduce the amount of virus in the blood to undetectable levels, meaning that you cannot pass on HIV.
Although widely used treatment is with anti-HIV drugs, which sometimes called combination therapy because people usually take three different drugs at the same time – often combined into one tablet. During pregnancy there is an effective treatment plan which is an set of infection control practices used to prevent the HIV transmission from the mother to the child, is known as Precautions and it must be taken to protect the baby’s health. It is also important to not share any used syringes, prevent any sexual contact with HIV-positive person without using protection. Diagnosis; it is crucial that the person exposed to the virus get tested through blood test to detect the earlier HIV. So the more likely the treatment will be successful
|
Q8 (6.1, 6.2)
- Explain how antibiotics function to control bacterial but not viral or fungal infections:-
Before the 20th century, there were no effective treatments for infections caused by bacteria, including pneumonia, tuberculosis, gonorrhea, rheumatic fever and urinary tract infections. But in 1929, bacteriologist Alexander Fleming discovered the first true antibiotic called penicillin, ushering in a new age of medicine that lead to a huge reduction in the number of human death. Antibiotics are the chemical substances which have the ability to kill disease causing microorganisms. Although antibiotics are derived from the bacteria, they are mostly used against bacterial infections. This is because these microbes release chemicals which can be used as weapons against other harmful microbes. There are also some antibiotics which are synthesized in the laboratory.
There are many different types of antibiotics that can be used depending on the infection a patient is suffering from. During the disease of cancer, the immune system cells become weak and body becomes susceptible to various bacterial infections. Antibiotics were prescribed to block these infections. Antibiotics only work against bacterial infections; they do not work against viral infections such as flu, measles, Aids and chickenpox because viruses are not the living microorganisms as they do not have ells structure or carry out biochemical process that can be targeted. However viruses have the ability to enter the host cells and reproduce their own DNA/RNA inside the cells as result to this the cells burst and destroy. The viruses have similar surface membrane to our cells so it is also difficult for our immune system cells to target. Also they have the ability to change their surface shape so the body won’t be able to recognize them if they enter again.
Since then, scientists have found dozens of antibiotics, which fight bacteria in a variety of ways. Many antibiotics, including penicillin, work by attacking the cell wall of bacteria. Specifically, the drugs prevent the bacteria from synthesizing a molecule in the cell wall called peptidoglycan, which provides the wall with the strength it needs to survive in the human body.
Other antibiotics prevent DNA replication in bacteria. As there is a class of antimicrobials known as quinolones targets DNA gyrase, which is an important enzyme that helps unwind DNA for replication. Ciprofloxacin and similar antibiotics effectively prevent the bacteria from multiplying by removing the enzyme gyrase.
Some antibiotics, including tetracycline, which is used to treat acne, respiratory tract infections and other conditions, are able to inhibit protein synthesis. The drugs do this by preventing key molecules from binding to selected sites on cell structures called ribosomes, where protein synthesis occurs. Without its proteins, the bacteria can’t carry out vital functions, including asexual reproduction (fission binary). Rifamycin, a group of tuberculosis-fighting antibiotics, achieves a similar effect by inhibiting the synthesis of RNA, a molecule involved in translating the body’s DNA into proteins.
Other antibiotics fight infections by stopping bacteria from producing folic acid — an important vitamin — or disputing the structure of a bacterium’s cell membrane, which controls how substances move in and out of the cell.
b) Explain the difference between bacteriostatic and bactericidal antibiotics:-
Antibiotics can be classified into two categories known as bactericidal agents and bacteriostatic agents, either one of these agents or a combination of these two can be used in order to treat an infection; it all depend on the type of the infection, growth conditions of microorganisms and the reduction rate of bacteria, and choosing the right antibiotic will depend on the mechanism of action of bactericidal and of bacteriostatic.
Bactericidal; Bactericidal agents are used to kill microorganisms by inhibiting the synthesis of cell wall. Therefore the number of microorganisms (bacteria) will decrease in the presence of bacterial agents so the microorganisms won’t remain viable. The bactericidal do not allow the immune system to deal with the infection as they directly kill bacteria. Usually, endocarditis and meningitis are treated by bactericidal drugs. Examples for bactericidal antibiotics include; penicillin derivatives, cephalosporins, monobactams, and vancomycin. The minimum concentration of bactericidal needed to kill bacteria is called ‘’minimum bactericidal concentration ‘’ or MBC. If the doses of bactericidal agents are low then they may act as bacteriostatic agents.
Bacteriostatic; Bacteriostatic agents are used to stop micrrooganisms (bacteria) from growing and replicating , this can be done by interfering with their protein production, DNA replication, or other aspects of bacterial cellular metabolism.. Unlike the bactericidal agents, the bacteriostatic agents must works together with the immune system to inhibit the microorganisms’ activities. So the bacteria do not die but they cannot grow or replicate either, this means that the number of microorganisms remains the same in the presence of bacteriostatic agents. According to drug concentration, the activity may differ; for examples, if a high concentrations of bacteriostatic agents is used, then they may act as bactericidal. In most urinary tract infections, it is recommended to use bacteriostatic antibiotics. The antibiotics include tetracycline, sulfonamides, spectinomycin, trimethoprim, chloramphenicol, macrolides and lincosamides are some examples for bacteriostatic agents. Minimum concentration of a drug that is needed to inhibit the growth of a certain strain of bacteria is known as ‘minimum inhibitory concentration’ or MIC.
References
Biology LibreTexts. (2018). 11.3E: Phagocytosis. [online] Available at: https://bio.libretexts.org/TextMaps/Map%3A_Microbiology_(Kaiser)/Unit_5%3A_Innate_Immunity/11.4%3A_Early_Induced_Innate_Immunity/11.3E%3A_Phagocytosis [Accessed 5 May 2018].
Cliffsnotes.com. (2018). Humoral and Cell-Mediated Immune Responses. [online] Available at: https://www.cliffsnotes.com/study-guides/anatomy-and-physiology/the-immune-system-and-other-body-defenses/humoral-and-cell-mediated-immune-responses [Accessed 5 May 2018].
Cliffsnotes.com. (2018). Phagocytosis. [online] Available at: https://www.cliffsnotes.com/study-guides/biology/microbiology/nonspecific-body-defense/phagocytosis [Accessed 17 May 2018].
Education.seattlepi.com. (2018). Functional Difference Between T Cells & B Cells. [online] Available at: http://education.seattlepi.com/functional-difference-between-t-cells-b-cells-4573.html [Accessed 5 May 2018].
Steane, R. (2018). Antibiotics. [online] Biotopics.co.uk. Available at: http://www.biotopics.co.uk/g11/antibiotics.html [Accessed 5 May 2018].
DifferenceBetween.com. (2018). Difference Between Bactericidal and Bacteriostatic | Bactericidal vs Bacteriostatic. [online] Available at: https://www.differencebetween.com/difference-between-bactericidal-and-vs-bacteriostatic/ [Accessed 5 May 2018].
Daniel Murrell, M. (2018). HIV and AIDS: Causes, symptoms, and treatments. [online] Medical News Today. Available at: https://www.medicalnewstoday.com/articles/17131.php [Accessed 5 May 2018].
University of Illinois-Chicago, S. (2018). Leukemia: Causes, treatment, and early signs. [online] Medical News Today. Available at: https://www.medicalnewstoday.com/articles/142595.php [Accessed 5 May 2018].
Healthline. (2018). Alcoholism: Causes, Risk Factors, and Symptoms. [online] Available at: https://www.healthline.com/health/alcoholism/basics [Accessed 5 May 2018].
Information, H., Overview, D., Causes, S., Diabetes, S., Center, T. and Health, N. (2018). Symptoms & Causes of Diabetes | NIDDK. [online] National Institute of Diabetes and Digestive and Kidney Diseases. Available at: https://www.niddk.nih.gov/health-information/diabetes/overview/symptoms-causes [Accessed 5 May 2018
Cite This Work
To export a reference to this article please select a referencing stye below:
Related Services
View allDMCA / Removal Request
If you are the original writer of this assignment and no longer wish to have your work published on UKEssays.com then please click the following link to email our support team:
Request essay removal



